Eligibility Process
Eligibility Process
Understanding the Eligibility Process
1. Introduction
The Eligibility Process is a multi-step journey aimed at determining exactly which healthcare services and interventions a patient is eligible for. This comprehensive guide offers a high-level overview of how these specific healthcare services, benefits, and treatments to which a patient is entitled are determined.
The Eligibility Process is a series of interconnected steps designed to ensure that the right patient receives the right care, at the right facility, and that this care is properly covered according to the rules set by the Social Health Authority (SHA). It's about moving from simply identifying a patient to confirming their precise healthcare entitlements.
1.1. Why This Full Process Matters
An accurate Eligibility Process is key to efficient, fair, and compliant healthcare delivery. It is crucial because it:
- Ensures Fair Access: Guarantees that patients receive services aligned with their entitlements and contributions.
- Prevents Financial Surprises: Provides clarity to patients and providers upfront, avoiding unexpected costs and disputes at the health care facility.
- Protects the various Health Funds: Safeguards the financial sustainability of the Social Health Authority and its constituent funds by ensuring proper claims and preventing unauthorised services.
- Promotes Compliance: Adheres strictly to national healthcare regulations and policies.
- Streamlines Care Delivery: Equips healthcare providers with immediate, accurate information, enabling quicker and more informed treatment decisions.
- Maintains Data Integrity: Creates a reliable, single source of truth for patient eligibility, reducing errors and duplication.
2. The Eligibility Journey: Step-by-Step Process
The complete Eligibility Process is a multi-step journey, with a number of workflows, each building up to the next. Here are the key workflows:
2.1. Step 1: Patient Search
This is the foundational first step. It's all about accurately identifying the patient. Our system looks up a patientʼs details from a central database for patient identities using unique identifiers (like National Identity Number) to retrieve the patient's verified information.
This is important as, without having accurate data on the patient, all subsequent checks are impossible or unreliable. It ensures we're building the entire eligibility determination on the correct individual's foundation.
2.2. Step 2: Benefits Coverage
Once the patient is identified, this workflow determines what general healthcare service categories (known as "sub-benefits") the patient is entitled to receive in a specific healthcare facility. It cross-references the patient's details with the details of the specific health facility.
This step is important as it establishes the scope of services the patient can access. It confirms which types of care this patient is eligible for at a facility.
2.3. Step 3: Intervention Coverage
Building on the general sub-benefits, this workflow refines the eligibility further to pinpoint the exact healthcare interventions (specific medical procedures) a patient is eligible to receive. It applies the Social Health Authority's (SHA) detailed rules, considering the patient's eligibility and the specific facility's licensed capabilities and contractual agreements with SHA for those interventions.
This is important as it is the level of detail needed for actual clinical decisions and accurate billing. It informs on what specific treatments can a patient receive at a facility. It prevents unauthorised procedures and ensures accurate tariff enforcement.
2.4. Step 4: Contribution Status
This workflow performs a financial health check of the patient's coverage. It verifies their current payment standing with the Social Health Authority (SHA) and assesses their status within any special schemes like the Public Office Medical Fund (PMF) for civil servants. It determines if their contributions are up-to-date and if they qualify for services based on their financial compliance.
It is important as it ensures that certain services are only provided to those who are current with their payments, safeguarding the fund and preventing financial loss for providers.
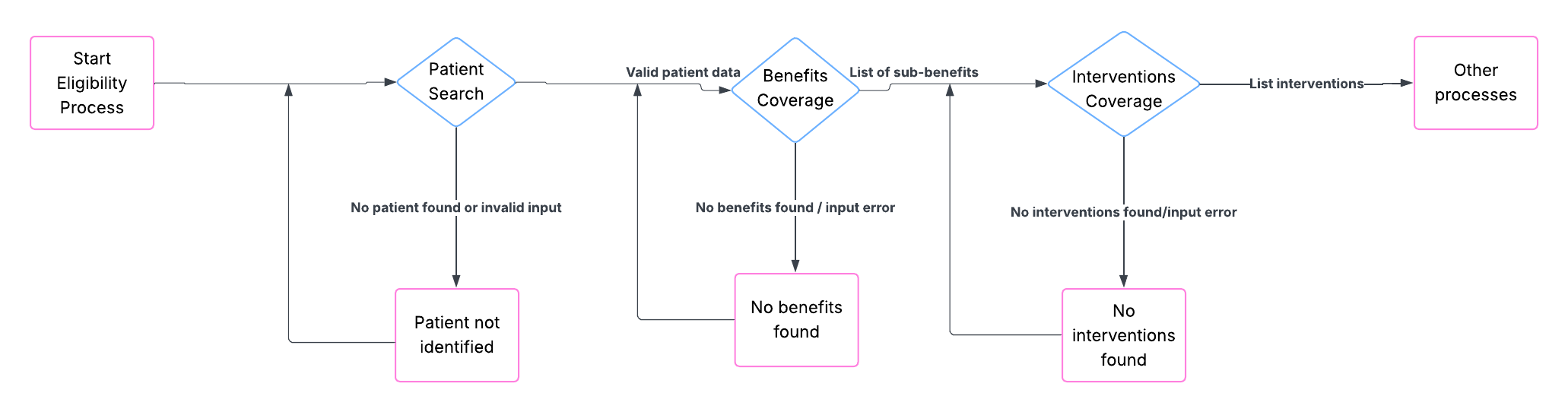
3. How Workflows Connect
While each workflow has a specific job, they are deeply interconnected. Data flows seamlessly from one step to the next, with crucial cross-workflow validations ensuring integrity:
- Single Source of Truth: Core patient data is always sourced from a central database via Patient Search, ensuring a consistent patient data across all subsequent checks. Similarly, facility data is validated against a central Facility Registry database.
- Cascading Dependencies: Each subsequent workflow depends on the successful completion and accurate output of the preceding steps. For example, if a patient cannot be found, no further eligibility checks can proceed.
- Consistent Identifiers: The patient and facility identifiers must be consistently passed and remain valid across all relevant workflows to ensure that all checks are performed for the correct individual and facility visited.
- Dynamic Rule Application: Information gathered from earlier workflows, like patient details, facility details, and contribution status, dynamically informs the SHA rules applied in later stages to determine precise eligibility.
4. Key Success Factors for Overall Eligibility Integration
For your integration with the entire Eligibility Process to be successful and efficient:
- Accurate Patient Identification: Ensure accurate patient details are obtained from a successful Patient Search. This is the foundation of the entire process.
- Validate Facility Data: Consistently provide correct and verified facility identifiers, as facility capabilities and contracts are central to benefits and interventions.
- Understand Interdependencies: Recognise that errors or missing data in an earlier workflow will inevitably cascade and cause failures or incorrect outcomes in later steps.
- Understand SHA Rules: Having a minimal understanding of how patient status, facility type, and contribution status influence eligibility will help you interpret results and troubleshoot effectively.
- Design for All Outcomes: Be prepared to handle all possible responses from our workflows (e.g., "Patient Not Found," "No Benefits Found," "Not Eligible Due to Contribution," "Input Error") and design your system to clearly communicate these to end-users.