Eligibility Process Guide: Intervention Coverage Workflow
1. Overview: Determining Specific Services
This guide focuses on the Intervention Coverage workflow, an important stage within the broader Eligibility Process. Building upon the patient identification and general sub-benefits determination, this workflow's primary role is to pinpoint the exact, granular healthcare interventions (e.g., specific medical procedures, medications, or diagnostic tests) a patient is eligible to receive at a particular health facility.
1.1. What This Workflow Does
The Intervention Coverage workflow retrieves a list of precise healthcare interventions available to a patient. It achieves this by combining:
- Verified Patient Details: The patient's comprehensive profile from the Client Registry, linked via their CR ID.
- Specific Facility Details: In-depth information about the health facility where the intervention would occur.
- Benefits coverage: A list of sub-benefits that the specific patient is eligible for.
Our system then applies the rules established by the Social Health Authority (SHA). These rules determine which interventions are covered based on the patient's eligibility (from previous workflows) and the facility's licensed capacity and contractual agreements with SHA.
1.2. Why This Workflow Is Critical
This workflow is paramount for precise and compliant healthcare delivery, preventing misinterpretations of general benefits. Its importance lies in:
- Preventing Unauthorised Services: Ensures that patients only receive interventions that are specifically covered and permissible for a given facility, avoiding non-compliance and potential fraud.
- Accurate Costing and Claims: Provides the exact codes for covered interventions, which are vital for accurate billing, claims submission, and financial reconciliation.
- Accurate tariff allocation: Given that tariffs are tied to the interventions, providing the right interventions ensures that the correct tariffs for the interventions are used.
- Optimising Patient Journey: Allows healthcare providers to immediately know what specific treatments they can offer, streamlining the patient's pathway and reducing administrative delays.
- Resource Allocation: Helps facilities manage their services efficiently by knowing what interventions are eligible for coverage through SHA.
In essence, this workflow moves from general "sub-benefits" to specific "interventions," acting as the final gate to confirm what can truly be performed and covered by SHA.
2. Workflow Details: Intervention Coverage
2.1. Workflow Description
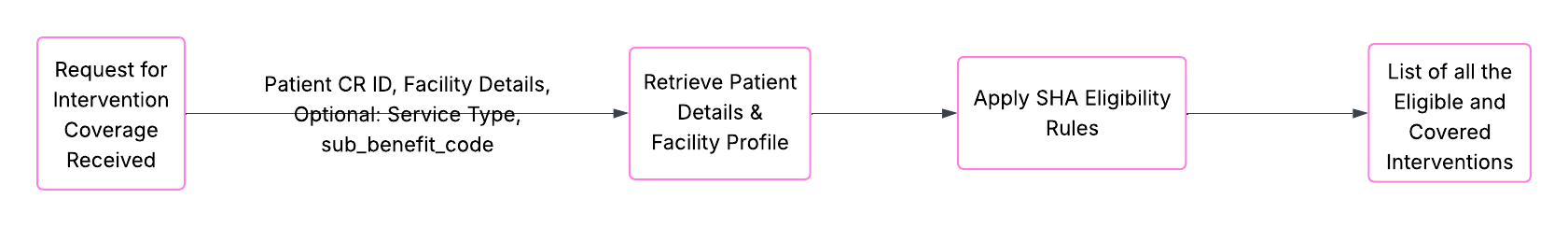
When a request for intervention coverage is received, our system executes an internal sequence:
-
Input Reception: The system receives the patient's unique Client Registry ID and the specific identification details for the health facility. It may also receive a broad service_type (e.g., "INPATIENT") or an optional sub_benefit_code if a more detailed check is needed.
-
Dependent Data Retrieval: Our system first ensures that comprehensive patient details are available (using the Client Registry ID) and then retrieves the complete profile of the specified facility (including its KEPH level, ownership, and contracted status). This relies on successful outcomes from previous workflows like Patient Search and facility data validation.
-
Rule Application (SHA Intervention Matrix): The system performs a multi-layered evaluation:
- It considers the patient's overall eligibility and specific sub-benefits determined in previous steps.
- It cross-references this with the facility's capabilities and its contractual agreements with SHA for specific interventions.
- It applies the Social Health Authority's detailed rules for benefits coverage, which might vary based on patient demographics, facility details and the services requested.
-
Intervention Determination: Based on the application of these rules, and the selected sub-benefit from the previous workflow, the system compiles a list of individual, covered interventions (e.g., "Appendectomy," "Malaria Test," "Specific Drug Prescription Code") that the patient is eligible for at that exact facility.
-
Outcome Delivery: The determined list of eligible interventions is prepared for use by the integrating system.
2.2. Key Validations: Our System's Essential Checks
These are the critical validations our internal system performs to ensure an accurate and successful intervention coverage determination. Understanding why these are in place helps you provide the correct information from your end.
Valid Facility Information (ID and Type) Must Be Provided:
- The system requires both a correct facility_id (the unique identifier for the health facility) and its facility_id_type (e.g., fr-code, registration-number).
- This is important as interventions are highly dependent on the facility's capabilities and authorisations. Our system needs precise facility identification to apply the correct rules about what specific procedures, tests, or treatments it is licensed and contracted to provide under SHA. Inaccurate facility data will lead to incorrect intervention lists.
Beneficiary Client Registry ID (CR ID) Is Mandatory:
- The patient's beneficiary_cr_id, obtained from the Patient Search workflow, must be provided.
- This ID is important as it is the primary link to the patient's full medical and eligibility profile. Without it, the system cannot access the patient's entitlements and apply the granular rules for specific interventions.
Facility ID Type Must Be a Valid Option:
- The facility_id_type must be one of the supported types recognised by our Facility Registry (e.g., fr-code, registration-number, fid).
- This is essential as it ensures the system correctly interprets and queries the Facility Registry for essential details needed to determine facility-specific intervention eligibility.
Patient Must Have a Valid Age and Gender:
- The patient's details retrieved via their CR ID must include a specified and valid age and gender.
- This is important as many interventions have age- or gender-specific eligibility criteria defined by SHA. For example, certain screenings are only for specific age groups. Missing or invalid demographic data will prevent accurate rule application for interventions.
Patient Records Fetched from CR only (not locally):
- The patient's data should only be from the Client Registry (CR) and not from any local database.
- This is important as it ensures that the Client Registry remains the ultimate "single source of truth" for patient biodata. It guarantees that our system always uses the most accurate and up-to-date patient information for benefit determination.
Facility Must Meet SHA Criteria (KEPH, Ownership, Contracted):
- The retrieved facility details must explicitly define its Kenya Essential Package for Health (KEPH) level, clearly indicate its ownership (e.g., government, private, faith-based), and confirm that it is formally contracted by SHA to offer services. These are essential in validating that the facility is allowed to offer services and be paid by SHA.
- These three attributes are absolutely important for applying SHA's rules. The KEPH level defines the scope of services a facility is equipped for, ownership can influence certain benefits, and being "contracted" confirms its legal standing to provide SHA-covered services. Without these, the system cannot accurately determine what interventions are valid at that specific location.
2.3. Workflow Data Dictionary
This helps show you the information we work with, whether it is required or not and in what format the system expects it in.
| Field Name | Description | Data Type | Required | Purpose |
|---|---|---|---|---|
| Beneficiary Client Registry ID | The patient's unique identifier was obtained from a successful Patient Search. | String | Yes | This is the patient's identity key. It ensures we are determining interventions for the correct individual and can access their full eligibility profile established in prior steps. |
| Facility Identifier | The unique identification number for the health facility where services are being considered. | String | Yes | This identifies the specific facility for the intervention. The facility's capabilities and SHA contracts are directly linked to this ID, fundamentally impacting which interventions are deemed eligible at that site. |
| Facility Identifier Type | The category or type of the Facility Identifier (e.g., fr-code, registration-number). | String | Yes | This tells our system how to interpret the Facility Identifier, allowing it to correctly query our Facility Registry and retrieve essential details needed for granular intervention determination. |
| Service Type | The broad classification of the healthcare service being considered (e.g., INPATIENT, OUTPATIENT). | String | Yes | This provides a broad context for the intervention check. While interventions are specific, their eligibility can still be influenced by whether they occur during an inpatient stay, an outpatient visit, or an emergency, guiding the application of certain SHA rules. |
| Sub-Benefit Code | (Optional) A specific code for a sub-benefit (e.g., "Dental Care"). If provided, the system will narrow its intervention search to within this sub-benefit. | String | No | This field allows for a more focused query. If you know the general sub-benefit category of the intervention you're looking for, providing this code can help the system return a more relevant and streamlined list of specific interventions, making the output more manageable. |
2.4. Expected Outcomes
- Successful Retrieval of Interventions: The system successfully identifies and returns a list of specific interventions (e.g., procedure codes, medication codes) that the patient is eligible to access at the given health facility, according to SHA rules and the facility's scope.
- No Interventions Found: The system indicates that, while the patient and facility are valid, no specific interventions could be found for the given criteria (e.g., the patient not covered for any service at that specific facility's level, or the requested service type has no corresponding interventions).
- Input Error: The system identifies that the provided input (patient ID, facility ID, etc.) did not meet our validation rules, preventing the intervention check from executing properly.
3. Critical Success Factors for Intervention Coverage Integration
For your integration with the Intervention Coverage workflow to be successful, keep these key points in mind:
- Accurate Input from Previous Steps: Ensure the beneficiary_cr_id and facility_id you're providing are correct and consistently validated from the Patient Search and Facility Registry, respectively. Errors in upstream data will cascade.
- Understanding SHA Rules for Interventions: While our system applies the complex rules, a conceptual grasp of how patient status and facility type influence specific intervention eligibility will aid in interpreting results and troubleshooting.
- Handling "No Interventions Found" Scenarios: Be prepared for situations where, even if a patient is generally eligible, no specific interventions are covered at a given facility or for a given service type. Design your system to clearly communicate such outcomes to end-users.